這次總統大選,讓很多美國人都在思考兩黨還有沒有可能合作。
如果從數百萬身患癌癥和其他疾病的患者角度考慮,我希望仍然有合作的可能。因為18年前,我罹患致命的非霍奇金淋巴瘤(NHL)時,兩黨合作幫我撿回了一條命。
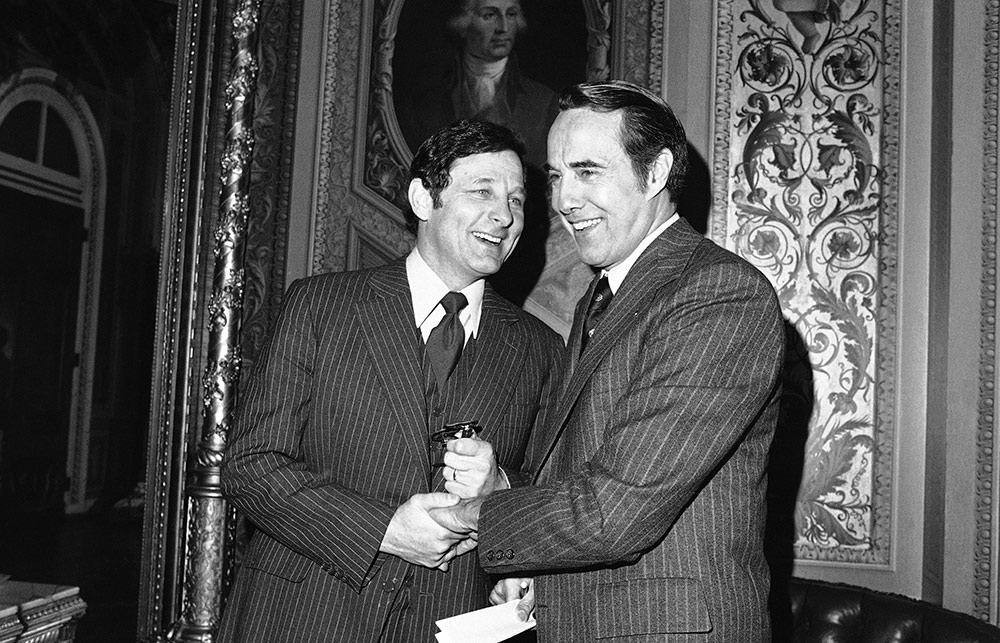
拯救我的藥物來自多年研究,但如果不是印第安納州民主黨人伯奇?拜赫和堪薩斯州共和黨人鮑勃?杜爾兩位參議員在1980年提出法律,研究成果就無法幫到我。
該項法律被稱為《拜杜法》(Bayh-Dole Act),允許大學、小企業和非營利組織擁有聯邦資助的早期發明專利權。相關機構可以將知識產權授權給有資源和經驗的私營公司,將有應用前景的創意轉化為能夠普遍使用的藥品。與私營部門合作很有意義,因為大學實驗室通常缺乏資源和人力,無力支持漫長昂貴的研究、測試和研發過程從而孵化創意。
在《拜杜法》之前,知識產權所有權均由政府掌握,偶爾轉化為實際產品向病人提供。當該法通過時,政府掌握發明中只有不到5%獲得商業生產許可。政府控制專利權期間,沒有一種藥物由聯邦政府支持的研發部門研發。
不過,幸運的是,參議員拜赫和杜爾暫時擱置黨派偏見,成功打破了僵局。具有里程碑意義的法律為私營公司搭建法律框架,后來推動200多項突破性的醫療創新,拯救我的創新就囊括其中。
2002年1月,我被診斷出非霍奇金淋巴瘤,是不治之癥,當時唯一的治療選擇就是化療。眾所周知,化療能夠減緩病程,但最終不可避免復發。當時,確診到死亡的平均壽命只有8年。得知無法跟丈夫一同老去,也看不到孫子孫女讀完小學,我心里非常難過。
然而化療并未減緩病情發展。治療了幾個月,該病的新療法及時上市,即放射免疫療法(RIT)。新療法跟化療不一樣,化療同時攻擊癌細胞和健康細胞,治療多達8次,RIT只針對癌細胞,而且只需注射一兩次。
2002年9月,我注射了兩劑最先進的RIT藥物替伊莫單抗,之后病情逐漸減輕,身體基本健康。如果不是醫療創新,我的生活可能遭遇非常不一樣的轉折。
替伊莫單抗治療方案中的關鍵部分是注入利妥昔單抗,該藥可以減少血液中癌性B細胞數量。斯坦福大學(Stanford University)的研究人員利用美國國家衛生研究院(National Institutes of Health)的資助,在20世紀70年代和80年代發現該種B細胞技術。
但將想法變成切實可行的治療方法需要大量時間和投資。如果不是當初研究人員離開斯坦福大學并于1985年成立Biotherapy Systems,進一步開發和商業化B細胞技術,醫學發現可能永遠沒有機會變成在商業上可行的癌癥療法。
僅僅一年后,Biotherapy Systems與IDEC制藥公司合并,成功實現了B細胞療法。產品經過多年調整,IDEC于1993年開始利妥昔單抗臨床試驗。到1995年,生物技術巨頭基因泰克(Genentech)與IDEC聯手實施微調。
1997年,美國食品與藥品管理局(FDA)終于批準,將利妥昔單抗的商標定為美羅華。
多虧1980年法律允許技術轉讓,否則該研究可能在斯坦福實驗室就已經夭折。正因為《拜杜法》的推動,私營部門才成功開創了市場化藥品。
我并不是唯一靠《拜杜法》支持的藥物創新系統救回一命的病人。根據該法律,私營公司能夠為病人提供數百種治療方法,包括癲癇藥物普瑞巴林、卵巢癌和乳腺癌藥物紫杉醇,以及多發性硬化藥物Tcelna等。
不過,目前社會活動團體正在向政客施壓,要求利用法律中從未使用過的條款奪取新冠藥物的專利權,這對私營制藥公司和患者都不是好消息。該做法并無法律依據,因為《拜杜法》只允許政府在極少數情況下獲得專利,比如當某家公司未廣泛提供產品時。盡管面臨各種壓力,立法者仍需合作,維持《拜杜法》的保護力度。
因為事關人命。
患者應該感謝參議員拜赫和杜爾,因為兩人認識到授權私營制藥公司將政府資助的研究轉化為藥物和療法無關黨派。后來提案在國會通過,當時羅納德?里根剛剛贏得大選,而吉米?卡特仍然在任。當年兩黨愿意攜手推動公共衛生,幫助跟我一樣與病魔抗爭的人,現在這種精神應該延續。(財富中文網)
貝齊?德帕里是病人利益代言人,也是《癌癥之地歷險記》(Adventures in Cancer Land)一書作者。
譯者:馮豐
審校:夏林
這次總統大選,讓很多美國人都在思考兩黨還有沒有可能合作。
如果從數百萬身患癌癥和其他疾病的患者角度考慮,我希望仍然有合作的可能。因為18年前,我罹患致命的非霍奇金淋巴瘤(NHL)時,兩黨合作幫我撿回了一條命。
拯救我的藥物來自多年研究,但如果不是印第安納州民主黨人伯奇?拜赫和堪薩斯州共和黨人鮑勃?杜爾兩位參議員在1980年提出法律,研究成果就無法幫到我。
該項法律被稱為《拜杜法》(Bayh-Dole Act),允許大學、小企業和非營利組織擁有聯邦資助的早期發明專利權。相關機構可以將知識產權授權給有資源和經驗的私營公司,將有應用前景的創意轉化為能夠普遍使用的藥品。與私營部門合作很有意義,因為大學實驗室通常缺乏資源和人力,無力支持漫長昂貴的研究、測試和研發過程從而孵化創意。
在《拜杜法》之前,知識產權所有權均由政府掌握,偶爾轉化為實際產品向病人提供。當該法通過時,政府掌握發明中只有不到5%獲得商業生產許可。政府控制專利權期間,沒有一種藥物由聯邦政府支持的研發部門研發。
不過,幸運的是,參議員拜赫和杜爾暫時擱置黨派偏見,成功打破了僵局。具有里程碑意義的法律為私營公司搭建法律框架,后來推動200多項突破性的醫療創新,拯救我的創新就囊括其中。
2002年1月,我被診斷出非霍奇金淋巴瘤,是不治之癥,當時唯一的治療選擇就是化療。眾所周知,化療能夠減緩病程,但最終不可避免復發。當時,確診到死亡的平均壽命只有8年。得知無法跟丈夫一同老去,也看不到孫子孫女讀完小學,我心里非常難過。
然而化療并未減緩病情發展。治療了幾個月,該病的新療法及時上市,即放射免疫療法(RIT)。新療法跟化療不一樣,化療同時攻擊癌細胞和健康細胞,治療多達8次,RIT只針對癌細胞,而且只需注射一兩次。
2002年9月,我注射了兩劑最先進的RIT藥物替伊莫單抗,之后病情逐漸減輕,身體基本健康。如果不是醫療創新,我的生活可能遭遇非常不一樣的轉折。
替伊莫單抗治療方案中的關鍵部分是注入利妥昔單抗,該藥可以減少血液中癌性B細胞數量。斯坦福大學(Stanford University)的研究人員利用美國國家衛生研究院(National Institutes of Health)的資助,在20世紀70年代和80年代發現該種B細胞技術。
但將想法變成切實可行的治療方法需要大量時間和投資。如果不是當初研究人員離開斯坦福大學并于1985年成立Biotherapy Systems,進一步開發和商業化B細胞技術,醫學發現可能永遠沒有機會變成在商業上可行的癌癥療法。
僅僅一年后,Biotherapy Systems與IDEC制藥公司合并,成功實現了B細胞療法。產品經過多年調整,IDEC于1993年開始利妥昔單抗臨床試驗。到1995年,生物技術巨頭基因泰克(Genentech)與IDEC聯手實施微調。
1997年,美國食品與藥品管理局(FDA)終于批準,將利妥昔單抗的商標定為美羅華。
多虧1980年法律允許技術轉讓,否則該研究可能在斯坦福實驗室就已經夭折。正因為《拜杜法》的推動,私營部門才成功開創了市場化藥品。
我并不是唯一靠《拜杜法》支持的藥物創新系統救回一命的病人。根據該法律,私營公司能夠為病人提供數百種治療方法,包括癲癇藥物普瑞巴林、卵巢癌和乳腺癌藥物紫杉醇,以及多發性硬化藥物Tcelna等。
不過,目前社會活動團體正在向政客施壓,要求利用法律中從未使用過的條款奪取新冠藥物的專利權,這對私營制藥公司和患者都不是好消息。該做法并無法律依據,因為《拜杜法》只允許政府在極少數情況下獲得專利,比如當某家公司未廣泛提供產品時。盡管面臨各種壓力,立法者仍需合作,維持《拜杜法》的保護力度。
因為事關人命。
患者應該感謝參議員拜赫和杜爾,因為兩人認識到授權私營制藥公司將政府資助的研究轉化為藥物和療法無關黨派。后來提案在國會通過,當時羅納德?里根剛剛贏得大選,而吉米?卡特仍然在任。當年兩黨愿意攜手推動公共衛生,幫助跟我一樣與病魔抗爭的人,現在這種精神應該延續。(財富中文網)
貝齊?德帕里是病人利益代言人,也是《癌癥之地歷險記》(Adventures in Cancer Land)一書作者。
譯者:馮豐
審校:夏林
This Election Day, many Americans are wondering whether bipartisanship is even possible anymore.
For the millions suffering from cancer and other debilitating diseases, I hope so. Because 18 years ago, when I faced a deadly diagnosis of non-Hodgkin lymphoma (NHL), bipartisanship laid the foundation that gave me my life back.
The treatment that saved me resulted from years of research that would have amounted to nothing without the law authored by two senators, Indiana Democrat Birch Bayh and Kansas Republican Bob Dole, in 1980.
Known as the Bayh-Dole Act, this law allows universities, small businesses, and nonprofit organizations to own the early stage inventions they make in the course of their research using federal grants. These institutions can then license their intellectual property to private firms, which have the resources and experience to turn promising ideas into widely available medicines. Partnering with the private sector makes sense, because university laboratories usually lack the resources and manpower to nurture ideas through the lengthy and expensive research, testing, and development processes.
Prior to Bayh-Dole, the government retained ownership of intellectual property rights, and only occasionally translated them into real-world products for patient use. At the time the law passed, fewer than 5% of these government-owned inventions were licensed for commercial production. And not a single drug was developed from federally supported R&D when the government took patent rights away from the inventor.
Fortunately, Senators Bayh and Dole set partisanship aside to fix this logjam. Their landmark legislation has helped create a legal framework for private firms to pioneer more than 200 groundbreaking medical innovations—including the one that saved my life.
When I was diagnosed with an incurable form of NHL in January 2002, my only treatment option at the time was chemotherapy. It was known to slow the disease’s progression but it would inevitably return. Back then, the median life span from diagnosis to death was just eight years. My heart broke, knowing that wasn’t enough time to grow old with my husband or see my grandchildren through grade school.
But chemotherapy didn’t slow the progression of my disease. A few months into treatment—and in the nick of time—a new type of treatment for NHL hit the market: radioimmunotherapy (RIT). Unlike chemotherapy, which attacks both cancerous and healthy cells and requires up to eight treatments, RIT targets cancerous cells only, and takes only one or two injections.
In September 2002, I received two doses of the cutting-edge RIT drug Zevalin and have been in remission and healthy ever since. Without medical innovation, my life might have taken a very different turn.
A crucial part of Zevalin’s therapeutic regimen is the infusion of the drug rituximab, a medication designed to reduce the number of cancerous B cells in the blood. Using grants from the National Institutes of Health, researchers at Stanford University unearthed this B cell technology in the 1970s and 1980s.
But it takes a lot of time and investment to turn good ideas into tangible treatments. And this discovery may never have become a commercially viable cancer treatment had those researchers not left Stanford and formed Biotherapy Systems in 1985 to further develop and commercialize their B cell technology.
Just one year later, Biotherapy Systems merged with IDEC Pharmaceuticals to take its B cell therapy across the finish line. After years of tweaking its product, IDEC kicked off clinical trial testing of rituximab in 1993. And by 1995, biotech giant Genentech joined forces with IDEC to fine-tune the drug.
Finally, in 1997, the FDA approved their drug rituximab under the brand name Rituxan.
Without the technology transfer process enabled by the 1980 law, this research could have died in Stanford labs. But because of Bayh-Dole, the private sector has created a market-ready medicine.
I’m far from the only patient who owes her life to the drug innovation ecosystem Bayh-Dole supports. Under this law, private companies have been able to bring patients hundreds of treatments—including the epilepsy drug Lyrica, the ovarian and breast cancer therapy Taxol, and the multiple sclerosis medication Tcelna.
Now, though, activist groups are pressing politicians to exploit a never-used provision of the law to seize patent rights for COVID-19 medicine, to the detriment of private drug companies and patients. There would be no legal basis for this course of action—Bayh-Dole only allows the government to grab patents in rare instances such as where a company is not making a product widely available. Still, with the pressure on, our lawmakers need to cooperate to keep Bayh-Dole protections strong.
Lives literally depend on it.
Patients owe a debt of gratitude to senators Bayh and Dole, who recognized that empowering private drug companies to turn government-sponsored research into usable medicines and treatments is not a partisan issue. Their bill found its way through Congress at a divided moment, when Ronald Reagan had just won election but Jimmy Carter was still in office. Their willingness to work together in the service of public health and patients like me should inspire us today.
Betsy de Parry is a patient advocate and the author of Adventures in Cancer Land.






